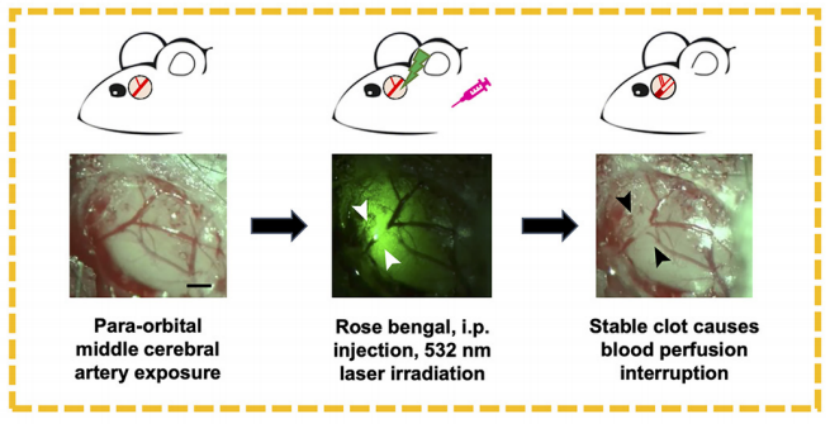
Photochemical-induced MCAO (in development)
Stroke, an acute cerebrovascular disease, is characterized by sudden brain blood flow disruption due to vascular occlusion (ischemic, 75%-90% of cases) or rupture (hemorrhagic). It manifests as focal neurological deficits (e.g., limb weakness, facial asymmetry, speech impairment) and is a leading cause of death and disability globally. Major risk factors include hypertension, diabetes, and smoking. The photochemical-induced middle cerebral artery occlusion (MCAO) model mimics ischemic stroke by triggering localized thrombosis via light-activated endothelial injury after photosensitizer injection. This model enables precise control of infarct size and is widely used to study thrombolytic therapies and neuroprotective mechanisms.
The photochemical MCAO model is induced by intravenous injection of a photosensitizer, followed by focal light irradiation through the intact skull over the MCA region. This triggers endothelial oxidative injury, platelet activation, and thrombus formation, mimicking human ischemic stroke. Zea-Longa and rotarod scores are used for neurological deficit analysis. TTC staining is used for quantification of infarct size. Laser speckle is used for assessment of cerebral blood flow. Morris water maze can be included as a behavioral test for cognitive impairment.
This method is ideal for studying thrombus formation mechanisms, evaluating thrombolytic therapies (e.g., clot-dissolving drugs), and exploring neuroinflammatory responses linked to post-stroke thrombosis. It enables precise infarct localization without craniotomy, facilitating investigations into blood-brain barrier disruption and inflammatory cytokine pathways. Additionally, the model supports pharmacological studies on herbal extracts or compounds (e.g., Verbena officinalis ethanol extract) that target thrombosis-related pathways. However, it lacks reperfusion phases, limiting its utility in ischemia-reperfusion injury studies compared to filament-based MCAO.
SCHEMATIC DIAGRAM
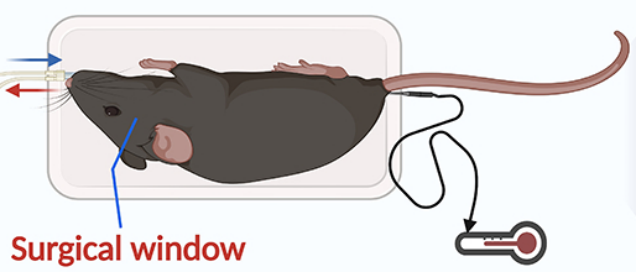
Mice are laterally positioned on a surgical platform, stabilized via incisor bar and tail fixation. Temporal muscle retraction with surgical tape enhances stability during craniotomy.
A craniotomy is performed over the squamosal bone to expose the MCA distal branch. Rose Bengal is intraperitoneally injected. After several minutes, a 532 nm green laser is applied to induce non-thermal thrombus formation, occluding the MCA without tissue heating, confirmed by intact perfusion in adjacent vessels.